When I discuss the concerns that you and your child have in one of my paediatric gastroenterology clinics, the clinical situation becomes clearer and often no further tests are needed.
In some circumstances though, and to help reach a diagnosis or exclude potential conditions, specialised tests can be used. These add more information to the evolving picture. Any investigations are carefully chosen and tailored to your child's specific situation.
There are various tests that are available to be used, including:
Blood tests - can be used to check for
- anaemia (when the body does not have enough healthy red blood cells and Haemoglobin - the protein that carries Oxygen to the body's organs)
- inflammation - usually the body's way of protection from injury or infection when short-lived, but if chronic (long-lasting) can lead to damage to various organs (including the gut for example inflammatory bowel disease)
- nutritional information including vitamin and mineral levels.
- kidney, liver and thyroid function
- the immune system is intact and functioning well
as well as to screen for and sometimes diagnose coeliac disease
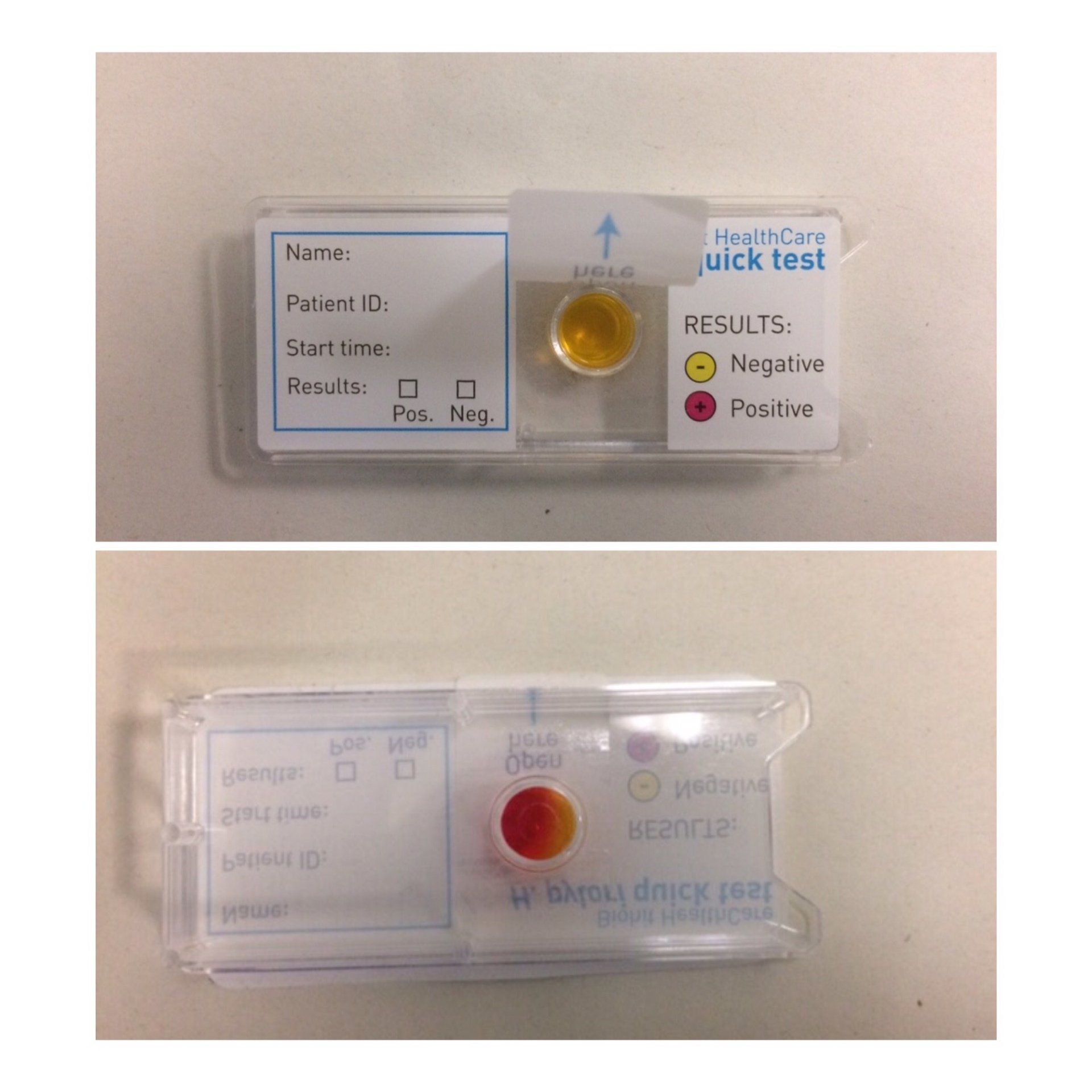
Stool or poo tests - to check for infections, gut inflammation and biochemical analysis in times of malabsorbtion.
Imaging tests such as x-rays, ultrasounds or other scans including MRI can be used to look at the bowel in greater detail. They can occasionally be helpful in estimating the gut transit time (gut motility studies) when difficult-to-treat constipation is a concern. Ultrasound and MRI scans can evaluate areas of the bowel or other digestive organs such as the gall bladder, liver, or pancreas for inflammation and the complications of inflammation.
Breath tests - can sometimes be used to check for carbohydrate intolerance such as Lactose or Fructose intolerance.
They can also check for excessive bacteria in the small intestine (small intestinal bacterial overgrowth SIBO), which can cause a variety of gastrointestinal symptoms including bloating and change in bowel habit, some of which overlap with irritable bowel syndrome.
They rely on the principle that gases such as Hydrogen (and in some Methane) are produced by bacteria in the bowel, that ferment poorly absorbed carbohydrates. Some of the gas produced is absorbed and eventually exhaled and can be collected and analysed.
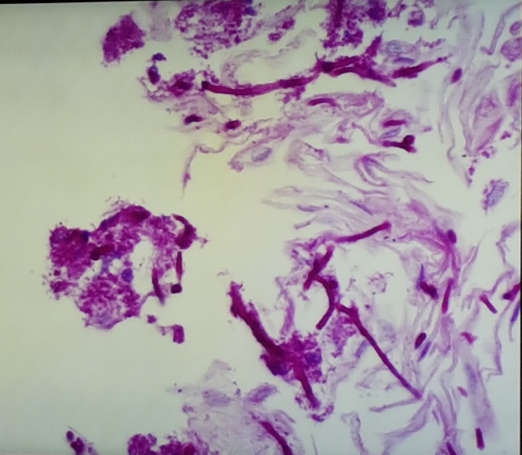
Paediatric Endoscopy and biopsy - can be used in some situations to look specifically at the lining layer (mucosa) of the digestive system in more detail.
An endoscopy is a procedure during which a trained endoscopist (e.g. a paediatric gastroenterologist, nurse endoscopist, adult gastroenterologist etc.) inserts an endoscope, a long thin floppy tube with a video camera and light at one end, into the digestive system via either the mouth or the bottom. High-definition Images during the procedure are displayed on a monitor in front of the paediatric endoscopist so that the lining layer of the gut can be seen clearly.
Whilst performing the procedure, Biopsy samples of tissue from the lining layer of the gastrointestinal (GI) tract are obtained for further detailed microscopic analysis by a pathologist.
This can be useful when searching for the cause of symptoms such as pain and bleeding or concerns with growth, swallowing or vomiting.
During the procedure, the naked eye of the endoscopist can see (macroscopic) changes such as ulcers or areas of redness that could possibly indicate inflammation. The biopsies allow for further analysis under a microscope by a pathologist, to check for the various types of inflammation involved, and for any (microscopic) changes that are not always visible during the procedure.