CASE STUDY - Abdominal pain in children
Tummy ache in a 12-year-old - chronic abdominal pain
We have all experienced abdominal pain or tummy ache at some stage or other. And if you're a parent, you'll also know, that tummy ache is something that most of our children have felt at some time.
It is one of the most common symptoms I see in my paediatric gastroenterology clinics.
Using some recent real cases I'll go through various causes of tummy aches in children. This is by no means an exhaustive list of causes, instead, I will highlight some of the more common reasons for abdominal pain in children.
In a recent clinic, my 12-year-old patient had been experiencing significant abdominal pain or tummy ache over a lengthy period of time. This was especially in the upper part of their abdomen and had also been feeling sick (nausea) for most of the time.
When I use the term chronic, I mean the prolonged length of time the symptom of pain has been present for, rather than the intensity or severity of the pain.
They had had some relief using some over-the-counter preparations but the situation had not improved enough. After meeting with the family, and from the initial consultation I found out that there had been a family history of stomach ulcers.
Peptic ulcer disease is a fairly common scenario within gastroenterology. Ulcers are sores within the gastrointestinal tract. When there is a break in the lining (mucosa) of the stomach or duodenum -the first part of the small intestine, they are known as peptic ulcers. The main symptom is abdominal pain. The examination may be normal although there may be some tenderness in the upper abdomen.
Ulcers occur because the usual defence mechanisms in place in the stomach or duodenum, are overcome by factors such as Helicobacter pylori or medications.
Together we decided to proceed with endoscopy as this test is diagnostic.
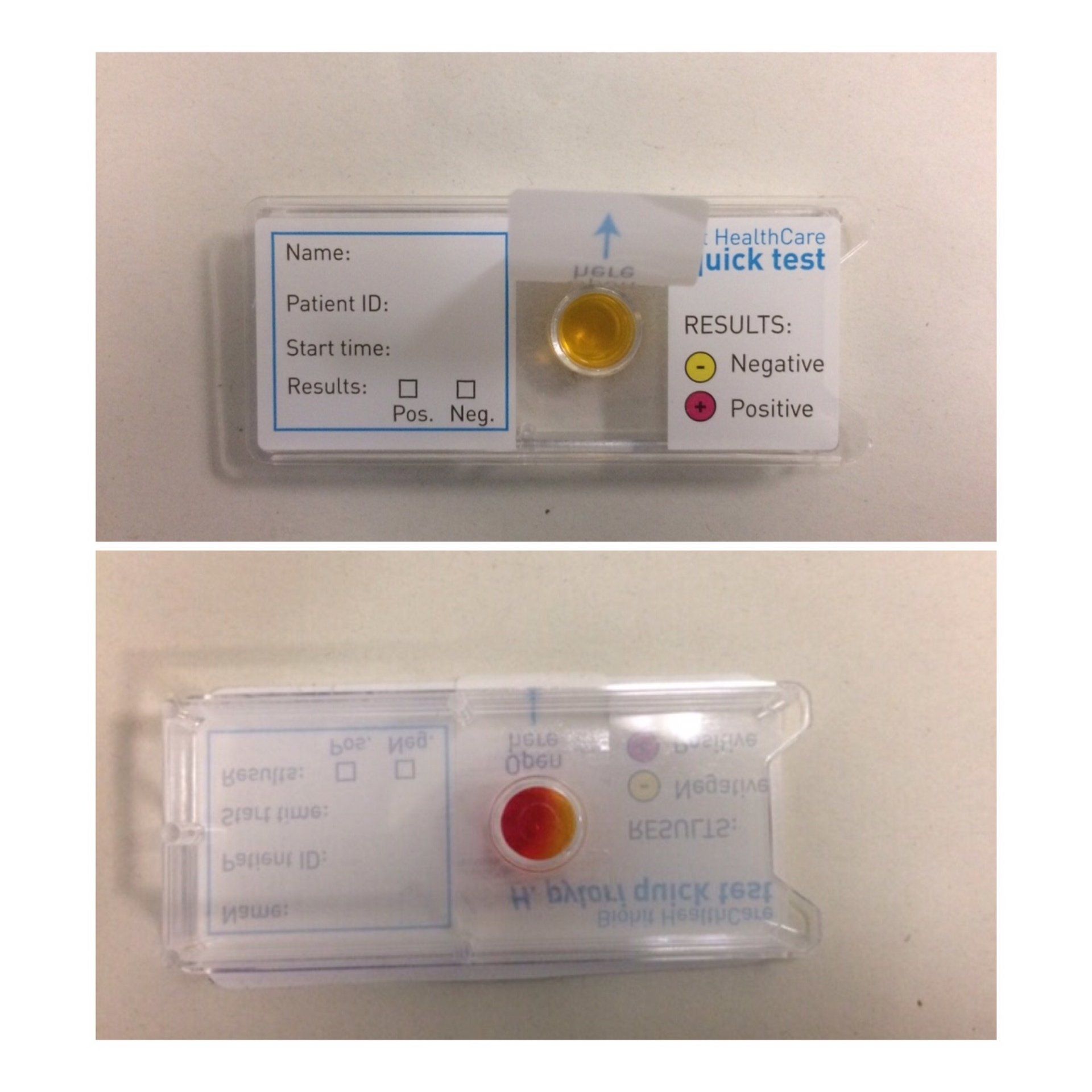
In this case, because of the relevant family history, during the endoscopy, another test, known as a CLO test was used. This helped to determine the cause to be due to Helicobacter pylori.
The image shows a CLO test kit used to detect the bacteria known as Helicobacter Pylori. During a paediatric upper GI endoscopy, a biopsy specimen from the stomach collected during the procedure is carefully placed in the little container shown. If Helicobacter pylori organisms are present, the colour changes from yellow to red. This test gives a rapid result often changing in just minutes.
The bacteria is commonly found in the stomach. Sometimes it may be found incidentally during the procedure and not be related to the original symptoms discussed during the consultation, that is to say it can be asymptomatic.
At other times It can be the cause of inflammation and sometimes ulceration of the lining of the stomach or first part of the small intestine e.g. a stomach or duodenal ulcer. This is known as peptic ulcer disease and can be a cause of abdominal pain and other symptoms such as nausea, vomiting sometimes with bleeding, and reduced appetite.
Treatment of Helicobacter Pylori is undertaken with the aim to improve symptoms but also to eradicate the bacteria.
A combination of antibiotics and acid suppression therapy such as Omeprazole, a Proton pump inhibitor, is used for approximately 2 weeks. Sometimes another test, a Helicobacter culture and sensitivity test - is used to determine the most effective antibiotics to be used, alongside the acid suppression therapy.
When considering this as a cause of symptoms it is important to discuss recent medication use with your paediatric gastroenterologist. Some medications, recent antibiotics or Omeprazole for example, may make it hard to reliably test for this bug.
The other major cause of peptic ulcers is the use of painkillers such as Ibuprofen or related medicines. This class of medicine, known as Non-steroidal anti-inflammatory drugs or NSAIDs for short are often used in the short term with no significant effect. However, when used over a longer period of time they can cause problems in the gut. Another recent patient I had seen had been using these regularly after a chest operation, and at an endoscopy performed for vomiting up blood with abdominal pain, was found to have several ulcers in the stomach.
How common is tummy ache in children and what causes it?
Tummy ache (Abdominal pain) is a very common symptom in children and can account for up to 5% of visits to a GP.
As the list of possible causes is very long, I like to break it down further into different categories.
Pain can be acute (of short duration) or chronic (lasting a long time - sometimes months).
Acute abdominal pain
When abdominal pain is of relatively sudden and short duration, or very severe, It is important to consider urgent situations such as appendicitis, digestive system issues such as intussusception (when one part of the bowel telescopes into another cutting off the blood supply), gall stones or stomach or duodenal ulcers for example.
In boys, testicle problems such as testicular torsion should not be forgotten as possible causes. This occurs when the testicle twists and its own blood supply is jeopardised, causing severe pain and potential damage to the testicle. It is a surgical emergency and is a cause of sudden pain that can also be felt in the abdomen before being more apparent in the groin.
In girls, ovarian issues such as cysts that twist or bleed, also need to be considered and acted on urgently.
These causes of acute abdominal pain are usually more short-term or sudden in onset. They may often have other more typical features (vomiting blood, being anaemic/pale) that raise alarm bells with a parent and medical practitioner and some of them may need surgical intervention.
It can still be difficult to distinguish between a particularly severe case of infectious gastroenteritis causing abdominal pain and some of the above conditions, especially appendicitis.
Chronic abdominal pain
For those in whom the pain is more long-standing, and occurs repeatedly, it is referred to as chronic abdominal pain.
In the vast majority, and in the absence of any alarm features (e.g Family history of stomach ulcers in the case above), often there is no significant or sinister underlying pathological condition to be found.
Despite this, there is no doubt that the tummy pain is real, and can sometimes be severe enough to have a negative impact on school attendance, children's activities and quality of life.
Some of the most frequent comments I hear from patients and families alike is that they feel people don't believe them about the pain. I'm sometimes told that they have been made to feel as though the pain is all in their head.
Recognising this pain is just as real and troubling as the pain from some of the other causes mentioned is a really important step.
An appropriate medical evaluation is an essential part of the process when assessing children with abdominal pain.
There can be a fine line between what is appropriate and what may be considered over-investigating and I'll go into more detail later.
How do paediatric gastroenterologists classify chronic abdominal pain?
The Rome Foundation, a group of internationally recognised experts in this area of gastroenterology (neurogastroenterology), has over the last two decades regularly produced diagnostic criteria around abdominal pain.
The latest criteria from 2016 can be found here.
Chronic abdominal pain in children can be broadly divided into the following categories
- dyspepsia - upper abdominal pain (approx. 7-8%)
- irritable bowel syndrome (IBS) - (approx 40%) pain associated with pooing and often a change in poo consistency or frequency
- abdominal migraine - often sudden intense pain that can be associated with nausea, vomiting or headache. Often lasts for a period of time and then your child may be entirely well again until the next bout occurs
- functional abdominal pain (not otherwise specified - approx 53%) when the pain may not be easy to fit into one of the 3 categories above
The terminology in this area of paediatric gastroenterology is changing and is moving away from words such as functional. This is because there has often been a stigma attached to this description.
The latest research in this area recognises the strong connections between the gut and the brain. The two are 'hard-wired' together so that factors that affect one often influence the other.
Did you know that there are as many nerve cells in the gut's nervous system as there are in the spinal cord? That is to say, there is a mini gut-brain !!
So now we refer to disturbances of this so-called gut-brain axis as the Disorders of Gut-Brain Interaction.
How do I evaluate a situation involving tummy ache in childen ?
It is very useful to be guided by the history given to me by you and your child, with a view to checking for any potential alarm features that would then prompt me to explore the situation further.
I will ask several questions regarding the pain including
- where it is - I often ask children to show me or draw on a diagram of their tummy
- what it feels like
- when it occurs
- how it starts and how long it stays for
- if it moves around
- any obvious triggers
- if there are any other associated changes or symptoms that occur at the time of the pain -for example, vomiting or diarrhoea
- if there has been significant weight loss
- the impact it has on day-to-day life for your child as well as the wider family
I will of course also carry out a clinical examination to check for any obvious concerning signs.
Other tests such as blood, poo, imaging tests (for example X-ray or ultrasound of the tummy) or less commonly endoscopy may be part of the evaluation. In the case earlier, as there was a family history of stomach ulcers, poo samples to check for Helicobacter and an upper GI endoscopy to have a look inside the stomach were appropriate.
Often though, in situations of chronic abdominal pain and no significant alarm features, the results from these tests can be quite normal.
I tend to try and aim for a one-stop shop of sorts when it comes to investigations so as not to find ourselves continuously pursuing an elusive cause.
It is not necessary to run every possible test for this reason. It is also important to avoid the situation arising whereby there is an incidental and usually harmless finding, that has had no influence on the pain, yet may then become an additional source of concern.
How to treat chronic abdominal pain
This depends on what is found during the assessment from the clinical history and examination.
In most cases of functional abdominal pain or more correctly Disorders of gut-brain interaction (DGBI), one may need to use a variety of approaches and these may include:
- Reassurance that no alarm features are present
- Explanation behind current research and thinking behind disorders of gut-brain interaction including
- the hard-wired nature of communications between our brains and our guts and visceral hypersensitivity
- checking for any trigger factors - these can be physical as well as social/ environmental and dealing with them e.g infections, lactose intolerance, bullying (or other stress factors)
- dietary modification e.g. the FODMAPS diet and IBS, see here for more information from the British Dietetic Association
- certain medications to help with
- spasm like pain
- modulation of the nerve pathways that carry the pain signals to the brain
Non-medical therapy
- Hypnotherapy is well recognised as being useful in the management of IBS for example
- cognitive behavioural therapy
- helping with coping strategies
- moving away from catastrophising assessment of events
- reducing the focus on the pain (less attention)
Unfortunately, there is often no instant cure for the pain, rather there may be a journey, during which different treatment strategies are attempted.
I hope you've found this a useful introduction to understanding tummy aches in children.
If you have a concern about your child's tummy ache and need some expert advice about it, please don't hesitate to be in touch.
You can contact the Kids Gastro Care team using the buttons on this page or calling 07956550446