About Dr Crespi Paediatric Gastroenterologist
Specialist help for tummy troubles in children from newborn to 18
With clinics in London and Hertfordshire
CURRENT ROLES
In 2023 after a 11 years as a Consultant at the Royal Free, I moved across London to take up a Consultant post at the Royal London Hospital, home to one of the largest paediatric gastroenterology units in the UK.
The possibility to encounter a diverse spectrum of gastrointestinal medical and surgical conditions and to join in an excellent multidisciplinary team was a great opportunity. As a lifelong learner, I look forward to a new challenge, stepping out of a comfort zone, with the growth and development this brings.
I am also keen to bring my experience, and innovative ways of doing things to the excellent team there.
Previous Roles
Royal Free Hospital London
I was a full time Consultant Paediatric Gastroenterologist and Endoscopist at the Centre for Paediatric Gastroenterology, Royal Free Hospital London from December 2011 through to 2023.
This included an almost 3 year period as an Honorary Consultant Paediatric Gastroenterologist at Great Ormond Street Hospital, through much of the COVID pandemic, whilst being the only full time paediatric gastroenterologist in the Royal Free paediatric gastroenterology team.
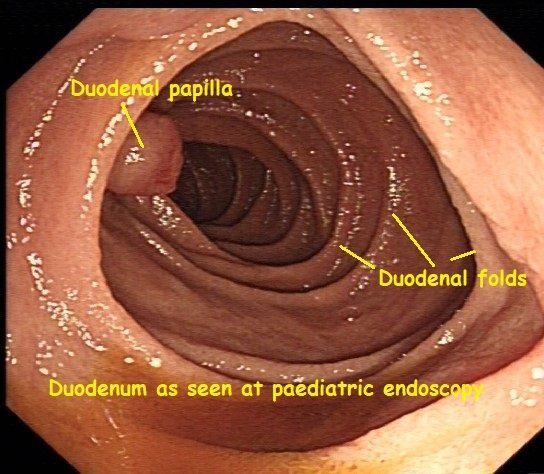
I have regularly carried out paediatric endoscopy procedures for patients from the Royal Free, both before the pandemic (weekly at the Royal Free) and then during the endoscopy recovery phase at Great Ormond Street with the fantastic team there.
I have always enjoyed being an endoscopy trainer helping trainee doctors both at the Royal Free and at Great Ormond Street develop their skills in this demanding technical skill.
Attendance at specialist paediatric and adult accredited endoscopy skills and other GI courses has always helped keep me up to date with the latest developments.
I love the interaction with colleagues from other specialties in both paediatric and adult medicine and allied healthcare in a clinical capacity, and when I was a member of the hospital's Drugs and Therapeutics Committee for several years.
Always eager to learn and develop, and at the same time apply a practical approach to a problem, to help reduce the endoscopy backlog, I recently collaborated with the dynamic, excellent adult and nurse endoscopist teams at the Royal Free. With their help I trained in the technique of Transnasal endoscopy or TNE.
With their support I recently used the TNE technique in the care of several of my older teenage patients from the Royal Free, having been inspired by meeting with colleagues already using TNE in the US and others in the UK who are also looking to use this in paediatric patients.
This is an exciting development in upper GI endoscopy, as it avoids the use of sedation or general anaesthesia and avoids stimulating the gag reflex, an unpleasant part of conventional endoscopy in adults. It provides excellent views of the lining of the food pipe, stomach and small intestine, as well as high quality biopsies, similar to those obtained during conventional upper GI endoscopy under general anaesthesia. It is also far less disruptive to school and work schedules as patients can be in and out of the hospital in an hour.
UCL Medical School
I am committed to training the next generation of medical students, and doctors within paediatric gastroenterology and was involved with lecturing and training medical students in paediatric gastroenterology over several years.
For a time I was also a Personal Tutor , acting in a pastoral supportive role to UCL medical students, and was an Honorary Clinical Associate Professor with the UCL Medical School in London.
Training in Paediatric Gastroenterology
I trained in the UK, having qualified in medicine from King's College, London in 2001.
I specialised in Paediatrics shortly after completing my first hospital 'House' jobs in Surgery, General Medicine and Intensive Care at King's College Hospital.
I then sub-specialised in Paediatric Gastroenterology, Hepatology and Nutrition and Paediatric Endoscopy.
I have been fortunate to have trained at some of the major paediatric gastroenterology, hepatology and nutrition training centres in London and the South East. These include: The Royal London Hospital, Chelsea and Westminster Hospital, King's College London and Southampton Children's Hospital.
I thoroughly enjoy training doctors helping them to improve their endoscopy and other clinical skills and still have an appetite to learn more myself.
MEMBERSHIPS and ASSOCIATIONS
- Fellow of the Royal College of Paediatrics and Child Health (FRCPCH)
- British Society of Paediatric Gastroenterology, Hepatology and Nutrition (BSPGHAN)
- BSPGHAN GI Motility working group
- British Society of Gastroenterology (BSG)
- Association for Child and Adolescent Mental Health (ACAMH)
SPECIAL INTERESTS
I see children with a wide range of digestive health issues and have up to date knowledge and
interests in several areas within the field of paediatric gastroenterology including:
- Chronic abdominal pain and Irritable bowel syndrome (IBS)
- Constipation and other GI motility issues such as gastro-oesophageal reflux
- Coeliac disease
- Eosinophilic Oesophagitis
- Food allergy and intolerance
- Peptic ulcers
- Paediatric inflammatory bowel disease (IBD) including
- Crohn's disease
- Ulcerative colitis
- Vomiting and swallowing problems including rumination syndrome
- Endoscopy - both conventional diagnostic paediatric endoscopy
- and innovative methods such as the use of Transnasal endoscopy in adolescents, helping to avoiding the need for sedation or general anaesthesia for upper GI endoscopy.
RESEARCH INTERESTS
I have had an active research interest in paediatric inflammatory bowel disease, with the long term aim of improving the quality of life and clinical outcomes in children with these chronic gastrointestinal conditions. More recently as part of the BSPGHAN motility group
PERSONAL
I'm kept pretty busy outside of work with my family and our Cocker Spaniel. I enjoy watching my beloved Spurs from time to time. It is far easier these days with Ange at the helm.

What does a Paediatric Gastroenterologist do?
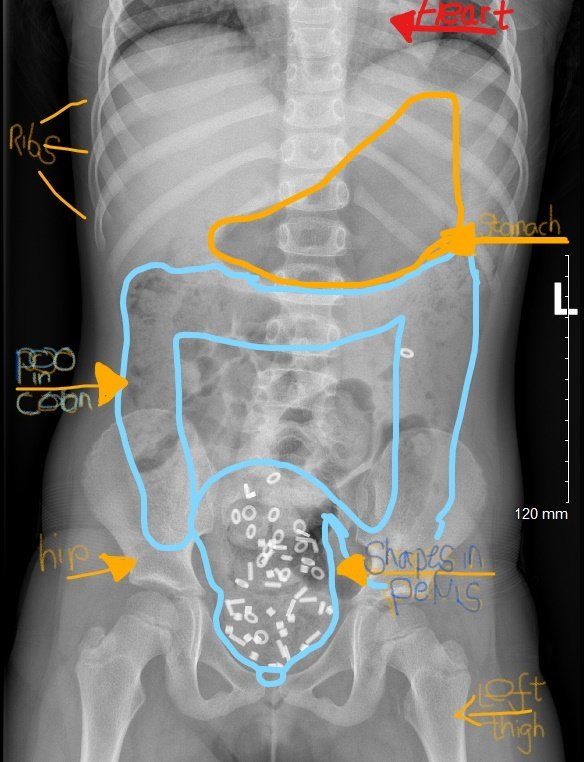
- diagnose and treat gastrointestinal symptoms and conditions affecting children and young people up to 18.
- if needed, carefully plan the use of specialised diagnostic tests and investigations including:
- blood tests
- poo (stool/faeces) tests
- imaging tests (x-ray or ultrasound)
- endoscopy and colonoscopy for children
Contact the Kids Gastro Care team
- links and videos on the Useful resources page
Video or Phone
consultations available
Caring
Thorough
Expert
Much Ado about Poo
Paediatric Gastroenterology clinics with Dr Daniel Crespi in London and Hertfordshire
- Royal Free Hospital London NW3 2QG, London, England, United Kingdom
- The Wellington Hospital Elstree The Waterfront, Elstree Borehamwood WD6 3BS United Kingdom
- Golders Green Outpatients and Diagnostics Centre NW11 9PY, London, England, United Kingdom
- Centennial Medical Care Centennial Medical Care, Elstree Borehamwood WD6 3 United Kingdom
Call us 07956550446
Email us contact@kidsgastrocare.co.uk
Email us
Business Hours
- Mon - Fri
- Appointment Only
- Saturday
- Closed
- Sunday
- Appointment Only






