Dr Daniel Crespi
How to diagnose coeliac disease in children

Hot off the press, in fact just published online ahead of print, are the latest European guidelines on how to diagnose coeliac disease in children
- to see a draft version click here.
Now you may have already known from my previous posts here in the
Much Ado about Poo Blog, and on the
Kids Gastro Care Facebook page
that Coeliac disease is fairly common and thought to affect 1 in 100 people. The mainstay of treatment remains total and life-long exclusion of gluten from the diet.
When and how does Coeliac disease present ?
Coeliac disease can affect anyone of any age provided that gluten has already been introduced into the diet. However, despite it being so common, it is still under diagnosed, possibly because of the many different ways it can show manifest.
From being asymptomatic (no symptoms to speak of) to a variety of gastro-related symptoms including
- tummy ache
- change in bowel habits (constipation or more often loose stools)
- abdominal bloating
- loss of appetite
- vomiting
- weight loss
- A negative effect on growth, children may not be growing as tall as expected for parental heights
- or they may not pass through the stages of puberty as expected.
- the skin with dermatitis herpetiformis
- the bones with relatively easily sustained fractures
- the blood system with difficult to treat anaemia.
- The liver may show changes (on liver related blood tests)
- very rarely the brain can be involved
- In women of childbearing age it can also be a cause of fertility related issues.
How does a paediatric gastroenterologist diagnose coeliac disease
The way coeliac disease is diagnosed in adults involves a combination of clinical history and examination, blood tests and endoscopy with biopsy samples from the small bowel. It is imperative to remain on gluten throughout the diagnostic process until it is complete as otherwise these tests are not accurate and there can be diagnostic confusion. See the brilliant
Coeliac UK website
for more details about this
here.
Until recently coeliac disease was diagnosed in a very similar fashion in children as well, that is to say a combination of symptoms, positive
blood tests and gut biopsies
obtained during an upper GI endoscopy.
In children it is important to remember that all endoscopy should ideally be carried out by paediatric gastroenterologists and the procedure is performed under general anaesthetic rather than the sedation used in adults. This has become the accepted standard of care for paediatric endoscopy and is how I do things at
Kids Gastro Care. For more about children's endoscopy please have a look at the
useful resources page on the Kids Gastro Care (KGC) website where you can find a child friendly video discussing this.
Blood tests
The blood tests involved measure an IgA antibody to an enzyme called Tissue Transglutaminase or tTG-IgA test for short. Alongside this test one should also always test for a blood protein called Immunoglobulin A (IgA) as deficiency in this protein can lead to so called false negative results when measuring tTG. Other blood tests are also used to confirm a diagnosis including endomyseal antibody (EMA) and in the last few years a genetic marker test that looks at specific markers known as Human leucocyte antigens or HLA DQ2 and DQ8 has also been used.
Now the TTG blood test is a highly specific and sensitive test, so that when negative it is pretty good at ruling out coeliac disease. If there is also IgA deficiency as well, the test is much harder to interpret accurately. When positive it is a pretty good indicator that something is up in the small bowel, the most likely cause being coeliac disease.
The gut biopsies
The biopsies are small samples of tissue taken from the innermost layer or lining (mucosa) of the small intestine. The first part of the small intestine or duodenum is where most biopsies are taken from.
Now if I can take you back to Biology lessons of distant memory, the small intestine is the major site of absorbtion of nutrients in the body. Damage to this highly specialised absorbtive area leads to loss of the villi or finger like projections where absorbtion takes place and throws the body into a state of malabsorbtion and development of symptoms of pain, diarrhoea, weight loss etc.
To reach the small bowel to obtain these biopsies, an upper GI endoscopy or camera test is necessary
How was coeliac disease diagnosed in children before the tTG blood test was available...
Pre-dating the development of the blood test that measures the levels of antibody to Tissue transglutaminase (tTG) in those children in whom coeliac disease was suspected biopsies were essential. So going back to the 1970s, children would undergo a series of 3 endoscopic procedures with accompanying gut biopsies.
- the first would be to demonstrate the damage and changes in the small bowel associated with coeliac disease whilst on a normal (gluten containing diet),
- the second to show the recovery of the small intestinal mucosa or lining once placed on a gluten free diet for period of time
- and then the third to show the damage sustained when the child was challenged again with gluten to 'prove' the offending trigger was gluten. OUCH! or OUCH X 3!!!
So whats new Doc?
Since the introduction of the TTG blood test, the process for the diagnosis of coeliac disease changed dramatically.
If a child was suspected of having coeliac disease because of symptoms, a family history, or other blood test findings such as persistent iron deficiency anaemia, they would have a blood test to screen for it. The test would measure tTG and if they had a positive result they would then always go on to have an upper GI endoscopy and a set of biopsies whilst on a gluten containing diet, to show the damage sustained by the small bowel to confirm the diagnosis.
2012... a move away from blood tests and biopsy for all
In children, until 2012 the same methods as described above, were used to diagnose coeliac disease in all children. That is to say in all children, blood tests and biopsies
from the small bowel collected during upper GI endoscopy were needed. For more information about these procedures see the
Useful resources page on the Kids Gastro Care website here
In 2012, this all changed. Given that the tTG test is such a good test for coeliac disease, in select cases it was deemed possible to diagnose the condition without need to resort to endoscopy and biopsy. The higher the result of the tTG test, the greater the certainty of coeliac disease changes to be found at upper GI endoscopy.
The no-biopsy approach from 2012 for some not all
The criteria to fall into this group of patients included a child with symptoms consistent with coeliac disease alongside a strongly positive tTG result, more precisely if it was more than ten times the upper limit of normal for the laboratory in which it was being measured. So in the Lab at the Royal Free Hospital London where I have
my clinics and endoscopy lists, if it was more than 60, in combination with compatible symptoms and as well as the 2 other blood tests mentioned earlier (EMA and HLA tests) being positive, then that combination would be enough to diagnose coeliac disease.
This approach, a non-biopsy approach, was suggested only in this specific subset of paediatric patients fulfilling these criteria and also if the family are happy to go along with it. In all other cases, for example, no convincing symptoms, an associated condition such as Type 1 diabetes and a high tTG, a weakly positive tTG result, or at family request, then all those children would still need a biopsy.
In adult gastroenterology, this no biopsy approach has not been adopted (yet ?? ) and is a controversial area.
Fast forward to 2019..more changes ahead
And now we are entering another new era in the diagnostic pathway for coeliac disease in children. This latest guideline from ESPGHAN, is now advocating a
Biopsy avoidance approach in a much wider group of children.
The inclusion criteria has expanded greatly. So from now on, this would apply not only for children with obvious symptoms and strongly positive tTG blood test results but even in those with no symptoms at all and a strongly positive tTG result. The guidelines also remove the need for testing for HLA DQ2 or HLA DQ 8 markers.
So to summarise these latest developments:
if a child is suspected of having coeliac disease for whatever reason (symptoms or no symptoms etc) then they may be able to avoid having an upper GI endoscopy and small bowel biopsies if they have a combination of a strongly positive blood test result for tTG along with a positive EMA result on a second blood test sample.
Pitfalls in diagnosis of coeliac disease
I can not emphasise these points enough as from my experience of hundreds of cases they are still not always considered when referrals are made.
1) Prematurely removing or significantly reducing gluten intake before a confirmed diagnosis
When gluten is removed from the diet prematurely before the diagnostic process is complete it can often lead to confusion around a diagnosis. The child is then subjected to a gluten challenge or reintroduction of gluten in order to complete the diagnostic process more accurately.
It is essential that there has been enough gluten in the diet and for a sufficient length of time prior to testing
so that the blood tests can be reliably interpreted. If in doubt a paediatric dietician can help review your child's diet to ascertain if sufficient gluten has been ingested.
2) Forgetting to measure Total IgA at time of other tests
Other causes of confusion include having IgA deficiency. This is a fairly common from of immune system deficiency especially in the Caucasian population. Approximately 1 in 600 people generally are affected and it is even more common in those with coeliac disease.
See the information leaflet from the
primary immunodeficiency UK charity here
for more information about selective IgA deficiency. In such a situation the standard tTG test becomes unreliable as it depends on there being enough IgA around.
What does a paediatric gastroenterologist do ? Specialist involvement in diagnosing coeliac disease
Being a specialist in the field I'm aware of these latest guideline developments at an early stage.
As with previous changes to disease specific and specialty guidelines, awareness of this new route to diagnosis will gradually increase over time among family doctors and my colleagues in general paediatrics. The guidelines suggest that diagnosis is made by a paediatric gastroenterologist. All of these points will be covered during a consultation with a
specialist in paediatric gastroenterology,
and as with all my consultations, shared decision making conversations are held with you and your child to work out the best next steps around managing the situation.
Should you find yourself in a scenario where coeliac disease is being suspected please make your doctor aware of these new guidelines and also ask for a referral to a
paediatric gastroenterologist.
Much Ado about Poo
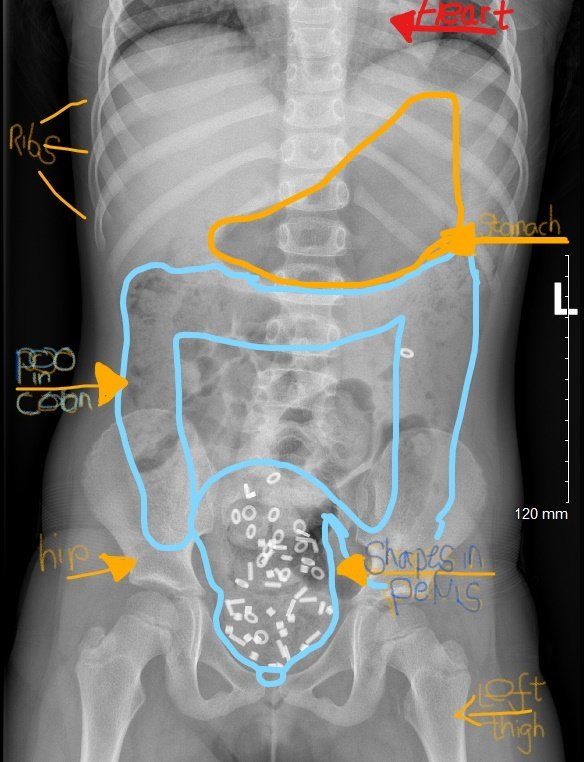
Constipation in children is a very common situation that I come across in my Kids Gastro Care clinics. The research literature often quotes a stat that up to 25 % of visits to a paediatric gastroenterologist are about constipation. Here I will discuss in some more detail, just one particular aspect of constipation in children, that of faecal incontinence or poo accidents. It is commonly associated with faecal impaction. For more on the diagnosis and management of constipation in children please click here. Being a 'poo doctor' I have become very used to talking about all aspects of bowel function and poo every day - just ask my kids! This isn't always the case for many others. There is still a great deal of stigma attached to poo problems in children and adults of all ages. One such area is around Poo accidents in children. Also called soiling, encopresis and faecal incontinence, it is not often the first thing that families talk about when I meet them in my clinics. In fact it may only come up when I directly ask about them. Poo accidents can be a tremendous source of upset, embarrassment, as well as social awkwardness, isolation and shame. They can leave parents frustrated at times as it is difficult to understand how their child can not seem to control their bowel motions. Sometimes children are told that they're being lazy and it can be easy to blame the child for the situation. I have seen children who needed upward of 8 changes of underwear and clothes a day because of poo accidents. Schools often send children home when these accidents occur. What should be fun childhood social activities such as swimming and sleep overs are limited or even stopped all together for fear of the dreaded accident happening. In the majority of children with poo accidents, the most common reason for this to occur is constipation. In some there is no significant constipation. I won't go into detail about that situation here in this post, as other aspects of care, often with a psychological emphasis, need to be addressed in greater detail. When there is a significant build up of poo within the large intestine (colon) or 'poo factory' as I call it, this is known as faecal impaction . Often the build up occurs in the very last section of the colon called the rectum - a sort of holding area for poo before it is passed out of the body. The impacted faeces sits in the colon and builds up gradually over time becoming more and more firm. Newer poo can sometimes slide past this mass of older poo, and slip out unannounced, as an accident. Sometimes this can be mistaken for diarrhoea. The rectum becomes more and more stretched over time. The usually sensitive rectum, loses its ability to sense being filled up with new poo as it has been stretched beyond its usual dimensions. Accidents can occur at any time, often seemingly without the child even noticing. To add to an already difficult situation, and because of the close location of the stretched rectum to the bladder, wee accidents can also become a part of the problem. Often this situation isn't recognised for what it is until late in the journey. A crucial early step is understanding what has happened and explaining how it has developed, using a non-judgemental, no blame approach. This combined with the right type of laxative treatment then aims to clear out - or disimpact - the old mass of poo that's been sitting there probably for some time. Occasionally, a special type of x ray of the tummy, a so called shape study (colonic transit study) may be used to help clarify the situation and visually demonstrate the build up of poo. The X ray picture at the top of this blog post, shows an accumulation of shapes in a mass of faeces in the pelvis,. This is in the last part of the colon with a stretched rectum. Other parts of the colon are also loaded with poo. The sensation of needing to go is weakened by this stretch of the rectum and so accidents occur regularly. The good news is that often dramatic improvements can be made when the situation is recognised and then managed appropriately with disimpaction . I have seen children go from having multiple accidents each day to none overnight, with a simple intervention using laxatives to clear out the impacted rectum . Disimpaction can either involve taking several days of oral laxatives in increasing amounts , or as an alternative more direct way, using 2 or 3 days of laxatives administered rectally - using enemas. Occasionally a combined approach is useful. Once this crucial first step has taken place, then a regular schedule of laxatives is needed to keep the colon clear and prevent a further build up. I really feel it's time to break down these taboos around poo and get this issue more widely recognised and then treated properly. Talking about poo with a fun down to earth approach is a start. It is only poo after all... If you think your child may be experiencing issues similar to those I have mentioned in this post, please do have a look at the Kids Gastro Care website for more information about constipation in children . If they're having troubles with their bowel control and you'd like to discuss things in more detail in an appointment with me, then please don't hesitate to be in touch and give us a call . The ERIC website , run by ERIC -the Childrens Bowel and bladder charity- is a fantastic resource for families affected by these issues. Please do help support their amazing work if you can by making a donation. I recently posted about this on our Facebook page with a request for donations for ERIC.
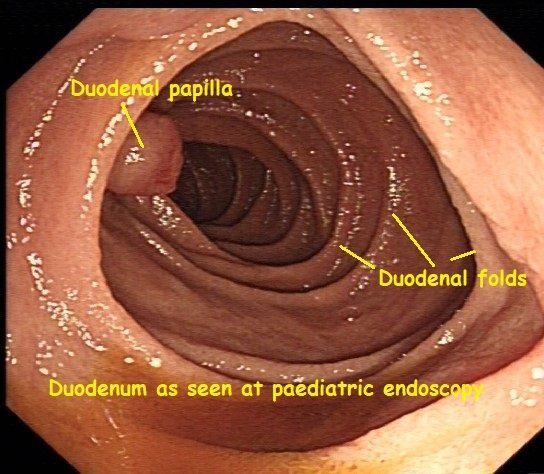
Every so often during my weekly paediatric endoscopy list, a striking image comes up on the screen, that makes me stop and reflect on the wonders of the human body. Here you can see a healthy-looking duodenum, from a recent paediatric endoscopy of the upper Gastrointestinal (GI) tract. This type of diagnostic endoscopy is also known as an Oesophago-gastro-duodenoscopy (OGD for short) or Gastroscopy. The duodenum, the first, and shortest part of the small intestine, derives its name from the Latin word duodeni. This refers to its length being approximately 12 finger-breadths. Partially digested stomach contents, in an acidic semi-fluid mass known as chyme, leave the stomach via the pylorus and enter the duodenum. Here further digestive processes take place. To help get your bearings with the image here, I'll explain a little more about some of the terminology and jargon used by an endoscopist. The central cavity of any hollow tube within the body is knows as its lumen. Having a good clear view of the lumen is essential during endoscopic procedures such as an OGD or colonoscopy. When trying to describe where a specific or noticeable feature or point of interest is during a procedure, and for ease of reference, endoscopists tend to compare the lumen of the bowel to a clock face. The protrusion visible at the 9 o'clock position, is the duodenal papilla. This is an important landmark seen during endoscopic procedures involving the upper gastrointestinal tract such as an OGD or ERCP. The latter is a specialised type of endoscopy used to look at the gall bladder, pancreas and their associated pipework (or ducts to be more formal). Digestive juices from the gallbladder and the pancreas are transported downstream via these sophisticated pipes (ducts) to just behind or upstream of the papilla. They are mixed together, then squirted through the papilla, into the lumen of the duodenum, to mix with the chyme and help with digestion. These digestive juices contain: - Bile salts that help emulsify fat - Pancreas enzymes to help digest food - Bicarbonate to neutralise the acidity of the chyme and protect the lining of the small intestine from acid damage. Anyone who has experienced the pain brought on by a gallstone lodged in some of the ducts draining the gallbladder or pancreas, can testify to the fact that it is almost impossible to stand during such an episode. Although less common in children, gallstones can occur and are associated with bowel conditions such as Crohn's disease. I couldn't help but think how fitting are the words of the blessing for good health "Asher Yatzar". "Blessed... who has formed man with wisdom and created within him many openings and hollow spaces. It is obvious and known before Your Seat of Honor, that if even one of them would be opened, or one of them would be sealed, it would be impossible [to survive and] to stand before You.” This is recited at times most of us take for granted, after going to the loo for a wee or a poo for example. There was just something about this image that made me recognise the importance of being grateful for simple things, such as all our pipes and tubes being in good working order. For more about common topics related to paediatric gastroenterology, digestion and endoscopy click here . And if you would like to meet to discuss a digestive problem your child has, please don't hesitate to be in touch by calling us or sending us an email .
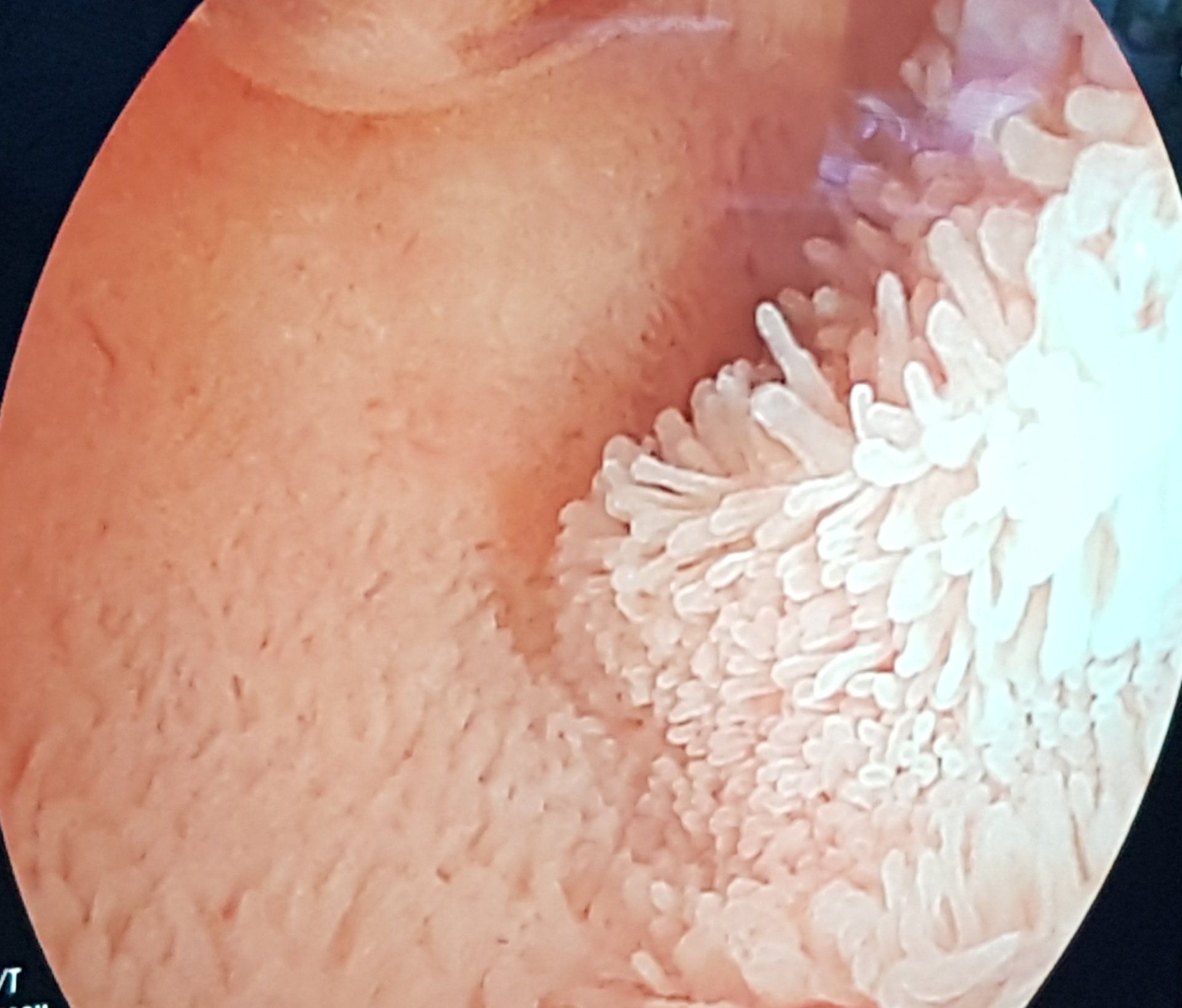
Every so often, I feel a sense of awe whilst at work. I came across this view during a specialised type of endoscopy (Double Balloon Enteroscopy or DBE) performed by a colleague, and I had that feeling again. Seeing a moving carpet of villi, the tiny finger like projections that coat the inner lining or mucosa of the small intestine in such detail, brought home to me the incredible workings of the human body, and how fortunate I am to be able to see this on a regular basis. Thousands upon thousands of these amazing structures help to hugely increase the surface area available for absorption of essential nutrients. including iron and vitamins. The small bowel can be affected by a variety of conditions that inflict damage to the villi. This impairs their ability to function so that one is at risk of malabsorption. Examples include Coeliac disease and Crohn's disease. Sometimes suspicion of the likely nature of the disease and it's involvement of the small intestine isn't enough. This is especially true when considering the use of potent medications that suppress the immune system, with the aim of healing the damaged areas. Having actual visual and biopsy proven evidence of involvement of this section of the GI tract can be crucial in deciding on the next steps in managing a condition. With most of its length, aside from the first and last few centimetres, being beyond the reach of standard upper and lower Gastrointestinal (GI) endoscopy, the small bowel has always been harder to investigate. Imaging using Barium with x rays is now rarely if ever used as other radiological techniques are available and also to avoid excessive radiation exposure especially in children. MRI of the small intestine gives a huge amount of information not only about the small bowel but also surrounding areas and organs. It is used in both children and adults. Ultrasound of the small intestine, in the right hands, can also give very useful information about the state of the small bowel particularly with regard to whether it is affected by inflammation in Crohn's disease. It is particularly useful in children as it avoids the sometimes claustrophobic feeling some can feel when in an MRI scanner as well as being faster and cheaper. Using Double Balloon Enteroscopy or DBE, it is possible to inspect the entire length of the lining of the small intestine. It allows the endoscopist to reach a lot further than a standard upper GI endoscopy or OGD does. The same is true of video capsule endoscopy (VCE), the miniaturised video camera within a swallowed pill, that takes thousands of images of the small intestine as it moves along it. In very simple terms, I think of the VCE as a reconnaissance of the area, scouting for anything abnormal. A form of window shopping, when I can only see the area of interest, however I can't sample what I see. With DBE one can both see and sample the lining with a biopsy and in some cases therapeutic techniques can be used. The VCE is often used as a screening investigation and then if needed, one can literally examine the depths of the small bowel with the DBE to obtain samples of tissue for examination under a microscope. The two techniques complement one another and along with other investigations, when put together like a jigsaw, help build up the bigger picture. Both techniques have their pros and cons of course and these are always discussed in detail before they are used. Carefully selecting the right test for the right patient is part of the challenge so as not to lead to any harm that could have been avoided. For more information and child friendly videos on endoscopy, have a look at the Useful resources page of the website.
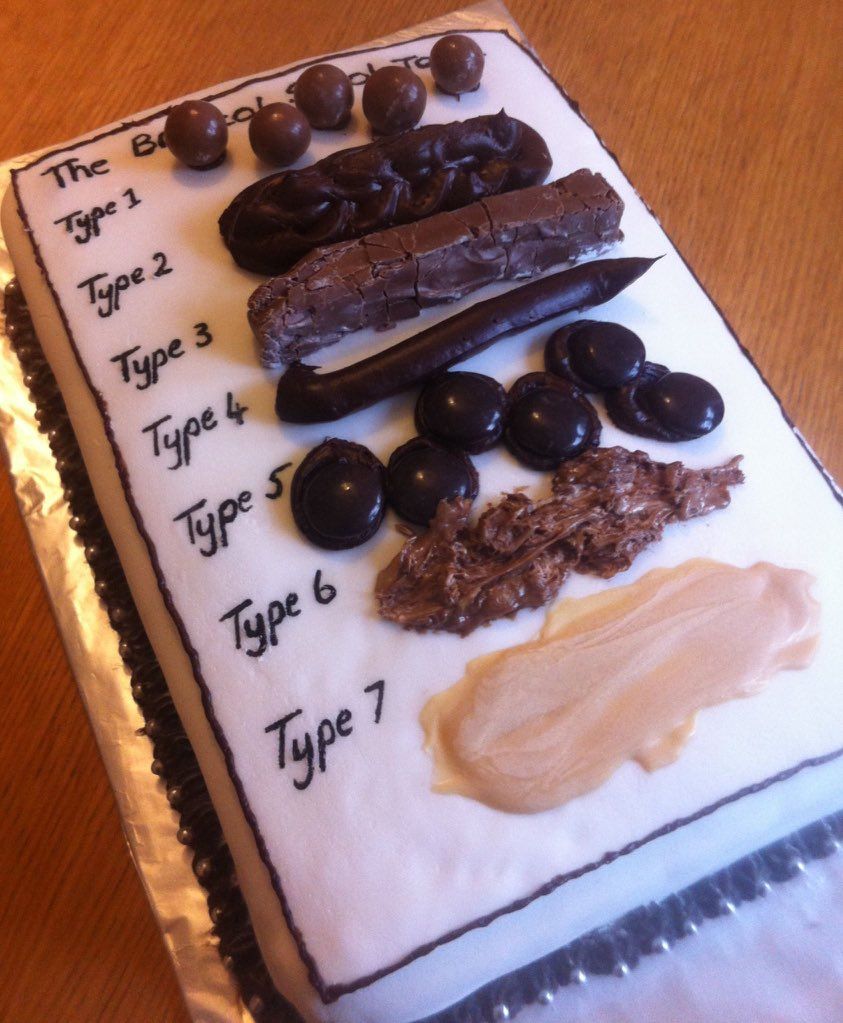
Good article on the BBC website discussing some research from King's College London. We talk about constipation in the paediatric gastro and nurse -led constipation clinics but are we actually talking about the same thing that patients are when we discuss it. Patients and their doctors and nurses should all be on the same page when it comes to defining what constipation is.
As a 'poo' doctor I make no apologies for getting into the nitty gritty detail about bowel habits in consultations to make sure I get a good understanding of the situation from the patient perspective. It's only poo after all. Breaking down the taboo further. A good read for all of us.
https://www.bbc.co.uk/news/health-48528058

It's a phrase one often hears.. 'follow your gut feeling' but what is that all about? Intuition or 'gut feeling' is something we all feel at different times. Some researchers from Florida State University have found that gut feelings are part of a protective system helping us to avoid running into trouble. Powerful gut to brain signals have a significant effect on our emotions and decisions. This is something I often talk about with patients...how the gut and brain are hard wired to one another and constantly communicating. It's a fascinating area with lots of research going on. This so called gut-brain axis has a significant role to play in many symptoms and conditions that are commonly seen in a gastroenterology clinic and offers another angle when it comes to formulating a treatment strategy. You can read more about it in the article published in the journal Physiology in 2018 authors L Rinaman and J Maniscalco. More on this in future posts.
A fantastic 2 day course run by the team at the Royal London Hospital. It covered all aspects of Neurogastroenterology. Studies show that a large number of GI outpatient consultations revolve around conditions within this subspecialty of gastroenterology. Understanding the mechanisms behind the development of these conditions allows for a more personalised treatment plan incorporating a biopsychosocial approach. (Image from D.A Drossman, Rome III (3) process , Rome Foundation).


